Spencer Wells
Weight Management Program Gives Spencer a New Life.
 On and Off the Field Spencer Wells entered adolescence as a typical “couch kid,” one of the estimated 12.5 million overweight American children and teens. “I was lazy pretty much of the time. Didn’t really do anything,” he recalls.
On and Off the Field Spencer Wells entered adolescence as a typical “couch kid,” one of the estimated 12.5 million overweight American children and teens. “I was lazy pretty much of the time. Didn’t really do anything,” he recalls.
His weight and lifestyle affected many aspects of his life, says his mother, Sheila Hughes. “He laid around the house. He had very low self-esteem. He didn’t do anything except go to visit a friend. A lot of his grades in school were D’s,” she says. “He didn’t start gaining weight until he was 6 years old. That is when his father died. When his father was alive, he was a well-balanced kid. We ate meals at home a lot. He did a lot of things with his father. They played football and basketball, and went swimming and fishing.”
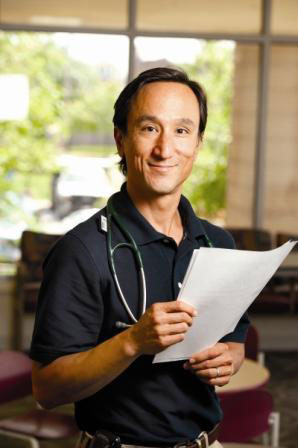 Spencer had been visiting SSM Cardinal Glennon Children’s Medical Center for many years, says Elizabeth Babusis, M.D., a member of the Pediatric Lipid Disorders Clinic. “I had to put him on medication for his cholesterol. That may be due partly to his genetics, but he was not really making progress. He wasn’t making changes in his food and exercise choices. I thought he needed an extra level of intervention.”
Spencer had been visiting SSM Cardinal Glennon Children’s Medical Center for many years, says Elizabeth Babusis, M.D., a member of the Pediatric Lipid Disorders Clinic. “I had to put him on medication for his cholesterol. That may be due partly to his genetics, but he was not really making progress. He wasn’t making changes in his food and exercise choices. I thought he needed an extra level of intervention.”
Babusis referred Spencer to the Live Right! weight management program at Cardinal Glennon Children’s Medical Center, where she also sees patients. The program combines input from pediatric specialists, psychologists and a nutrition counselor to deal with obesity and the many adverse health effects it can present.
 The incidence of obesity among children and teens has nearly tripled since 1980, according to the U.S. Centers for Disease Control and Prevention (CDC). Approximately one in six children and teens in the United States is obese based on measurements of body mass index (BMI). The index is calculated through age-adjusted comparisons of weight and height.
The incidence of obesity among children and teens has nearly tripled since 1980, according to the U.S. Centers for Disease Control and Prevention (CDC). Approximately one in six children and teens in the United States is obese based on measurements of body mass index (BMI). The index is calculated through age-adjusted comparisons of weight and height.
CDC statistics show that the growing incidence of obesity has brought increases in harmful effects such as high blood pressure, high cholesterol, Type 2 diabetes, sleep apnea, asthma, liver disease, gallstones, heartburn and musculoskeletal pain and deformities. Overweight youth also face great risks of social and psychological problems such as poor self-esteem and depression.
Obesity and all of its side effects can linger into adulthood. “There used to be an attitude that children would grow out of obesity,” says Babusis, an adjunct assistant professor of pediatrics at Saint Louis University School of Medicine. “When we look at the statistics over time, we see that they don’t grow out of it. If you have excess weight in childhood, it is more likely you are going to have excess weight in adulthood, along with all the problems that come with it.”
Obesity-linked diseases that once were rare in childhood are now seen routinely, says Nadim Kanafani, M.D., director of Live Right! and a pediatric endocrinologist at Cardinal Glennon Children’s Medical Center.
“Kids now have diabetes and obstructive sleep apnea. We have documented cardiovascular disease as early as 3 or 4 years of age in obese children,” he says. “Some of the children in our weight management program weigh 80 pounds by the time they are 3 years old. We have a 9-year-old who weighs 320 pounds, and a 16-year-old who is nearly 500 pounds.”
According to Kanafani, an assistant professor of pediatrics at Saint Louis University, two trends have created one of the biggest health issues facing pediatricians in the 21st century. “Over the last 30 or 40 years, the American diet has become increasingly layered, complex and processed. The availability of low-cost, high-energy, poorly nutritious food has increased and people consume it in large quantities,” he says.
Young people also are getting less exercise because there are fewer opportunities to play outside and more temptations to sit before television and computer screens. “Physical activity has been de-engineered from our days,” he continues.
The average school-age child or teen spends 7.5 hours a day using entertainment media such as televisions, computers, video games and cell phones, according to the CDC. The centers also believe that only 18 percent of high school students meet the recommended minimum of 60 minutes of aerobic exercise each day. With these trends, a new term, “obesogenic,” has emerged to describe the environments in which some children gain too much weight, Kanafani says.
 Three keys to weight management
Three keys to weight management
The Live Right! weight management program includes monitoring and treatment for the medical conditions associated with obesity as well as the nutritional and psychological guidance needed to help children lose weight. “Even younger children who are overweight can have trouble getting around and keeping up with their peers,” Babusis says. “Obesity can harm bones that are growing at a rapid rate during childhood. We can see crush injuries in the knee area that will cause the lower legs to grow crooked.”
Poor dietary choices also produce constipation and, paradoxically, malnutrition. “Large amounts of calories consumed are not necessarily nutritionally important calories,” says Babusis. “We can see problems with vitamin D deficiencies, which can limit calcium uptake, and that relates directly to bone health.”
Kathleen Spranaitis, P.N.P., B.C., of the division of pediatric gastroenterology is a pediatric nurse practitioner who sees patients in Live Right! “Children who are overweight frequently have gastrointestinal problems such as acid reflux, constipation and fatty liver disease,” she says.
Obesity is often accompanied by a diet lacking in the healthy fiber of fruits and vegetables, she says. “Some families, because they have low incomes or because both parents work, can’t always have fresh produce or cook healthy meals. They are doing all they can to get food on the table for their kids.”
Children who visit the weight management program often suffer from the same dietary issues that plague their parents. “Our kids often have one or more parents who also have weight issues. The parents are eating in the ways they were taught, and the kids will eat the ways they are taught,” Spranaitis says.
 A family’s first visit to Live Right! begins with a session led by registered dietitian Kathryn Helling, R.D., at which a healthy lunch is served with samples of light and nutritious foods. Many American families lack information on healthy food choices and appropriate portion sizes, Helling says. “We see families eating a lot of calorie-dense foods like snacks and cookies, that are not as nutrient-rich as fruits and vegetables. They need information on how much nutrition a toddler, a school-age child and a teenager need.
A family’s first visit to Live Right! begins with a session led by registered dietitian Kathryn Helling, R.D., at which a healthy lunch is served with samples of light and nutritious foods. Many American families lack information on healthy food choices and appropriate portion sizes, Helling says. “We see families eating a lot of calorie-dense foods like snacks and cookies, that are not as nutrient-rich as fruits and vegetables. They need information on how much nutrition a toddler, a school-age child and a teenager need.
“In families with weight issues, portions are usually very large. That reflects our social environment. We can go to the gas station and buy a 64-ounce soda or go to the movie theater and pick up a tub of popcorn that holds well over 1,000 calories. That is what they are used to. When we go over food models and a sample meal plan of what a child should be eating at a certain age, families are often quite surprised,” Helling explains.
To depict the empty and harmful contents of popular foods, Helling shows families a series of test tubes representing the fat content of items such as an order of french fries. She also wields a poster titled “Portion Distortion” that illustrates the
difference between a typical hamburger-with-fries meal and the much smaller
portions that would be appropriate for a child – and an adult.
According to a study recently published in the Journal of the American Dietetic Association, the leading sources of calories for children were cakes, cookies, doughnuts, pies, granola bars, pizza and soda. For 2-and-3-year-olds, the second leading source of daily calories was fruit juice. The CDC says sugared drinks are the largest source of added sugar and a major source of calories in the diets of American youth. On a typical day, 80 percent of children and teens consume a sugared drink. “Sugar-sweetened beverages are usually something we need to target when we are talking with a family,” Helling says.
Many parents mistake fruit juice as a healthy choice when in fact it contains as many calories as other sweetened drinks such as soda. “I encourage kids to drink no more than four to six ounces of 100-percent fruit juice a day,” Helling says. “Anything beyond that is excess calories. The kids can get better nutrition and fiber from eating the fruit itself.”
Helling advises healthy meal planning as a benefit for the entire family. “Parents can help to prevent obesity by role-modeling healthy eating habits themselves. They should sit down and have three meals a day. They can get their kids involved in meal preparation. Repeated exposure to healthy choices is important,” she says.
 A visit to the Live Right! clinic includes a talk with one of its two child psychologists, Joel Nadler, Ph.D., or Amy Ford, Psy.D. “We see low self-esteem, teasing by peers or bullying and sometimes depression,” Ford says. “It is unclear whether these issues cause or result from being overweight, but if a child is overweight, he can be teased and can have low self-esteem. Then he feels depressed and turns to food to cope.
A visit to the Live Right! clinic includes a talk with one of its two child psychologists, Joel Nadler, Ph.D., or Amy Ford, Psy.D. “We see low self-esteem, teasing by peers or bullying and sometimes depression,” Ford says. “It is unclear whether these issues cause or result from being overweight, but if a child is overweight, he can be teased and can have low self-esteem. Then he feels depressed and turns to food to cope.
When children turn to food to feel better, that adds more pounds and makes them feel worse about their weight, which unfortunately continues the cycle.”
Ford feels that the first goal of counseling is determining whether a child has behavioral or psychiatric issues that must be addressed in weight management treatment. “The child may be extremely depressed or having significant peer problems or difficulties at home or school. We work on coping skills if those things are happening. If the child is very oppositional or defiant, we help the parents with ways of managing that as well as giving the child skills to cope with whatever is making him angry or upset,” she says. “The child may have untreated attention deficit hyperactivity disorder, which makes them impulsive. If they see food, they want it and eat it.”
Food also may have become a means of quieting tantrums or winning compliance with other behavioral issues. “Goals should be recognized with nonfood rewards,” Ford says. “Give them extra activities or privileges instead.”
As with nutritional guidance, she says, the program’s behavioral counseling stresses family participation. “We encourage change within the whole family to be supportive of reaching the child’s goals. We don’t want the child to feel as if he has to eat healthy because he is being punished,” Ford says.
Also, she says, “One of the major psychosocial factors in childhood obesity is family lifestyle choices. Children fall into the same activity and eating habits as their families. Parents need to think of what their behavior is modeling to their kids.”
The most important contribution of the Live Right! team’s members may be encouragement. “We are all coaches and cheerleaders,” Spranaitis says. “We reinforce the eating and activity behaviors the others are suggesting. We give it our best shot.”
“I usually start discussions with parents by telling them that childhood obesity is not a child problem,” Kanafani says. “No child wants to be obese. Children are placed in environments that are obesogenic. Parents control the nutritional and activity environments in the home. Children do not have the ability to make choices. They will eat junk food if it is there. They will sit in front of the television all the time if it is on.”
Encouragement, Ford says, must be given in realistic doses. “We give them room for error. I tell families they should never set seven-day-a-week goals. If you want your child to watch less TV or eat more vegetables, doing that five or six days a week is fine. It is too hard if you set unreasonable goals, because it feels terrible not to meet them, and that often gets people off track.”
Taking the next step
Minimizing the nation’s obesity issues will require action in many areas, Kanafani says. “Systemic, multi-level changes will be needed, everything from food policy and food supply to the ways we build our neighborhoods.”
Kanafani hopes to expand the Live Right! program to provide a greater depth of service to the medical center’s patients and surrounding communities. “We have a strong team of people who are very experienced in caring for families struggling with severe obesity. I would like to expand our model to focus more on the complications of obesity and on nutritional education, and provide structured and supervised exercise opportunities.”
Kanafani’s vision for the next phase of weight management would include a nutritional learning lab. “Parents would come in and have more in-depth sessions with our dietitian on planning meals, shopping, reading labels and cooking. We could do hands-on learning with different foods, cooking styles and taste-testing,” he says.
An exercise physiology lab would fill the requests of parents who desire assistance in supervising their child’s needed activities. “We could collaborate with our folks in physical therapy and athletic training to do monitored, group-exercise sessions,” Kanafani says. “Parents are not sure how to encourage big kids to move and exercise safely.”
The center also would provide opportunities to study obesity complications and treatment outcomes, he says. “I am excited that the Cardinal Glennon Children’s Foundation is expressing interest in working with the program and possibly helping us expand.”
 The New Spencer
The New Spencer
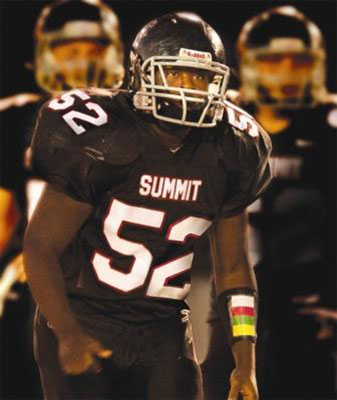
Spencer Wells has become a muscular athlete in the two years that he has been visiting the Live Right! clinic at Cardinal Glennon Children’s Medical Center. He now looks like he could be a football player – and he is.
Spencer is a junior at Rockwood Summit High School and a member of its football team. In the spring, he may once again be a member of the track team, specializing in the shot put and discus.“I am very happy for him,” Babusis says. “His success resulted from him deciding that it was time to act. Then he stayed with it. When we have a successful patient, it is because the child or parent decides to make changes. When there is willingness for change, we can have success.”
“It is a real challenge to reach and maintain a healthy weight,” Spranaitis says. “It is tough, really tough. It depends upon how committed the child and the family are.”
“The people in the clinic showed me how to change my diet and increase my activities,” Spencer says. “I’ve changed what I eat, the portions I eat and how it is made. I’m not eating fried foods. Instead I’m eating baked and grilled foods. It was pretty easy. I have longer hours of exercise, and I am able to perform longer in sports. Now I have to stay active. I’m used to it.”
Spencer’s life has improved off the athletic field, too, says his mother, Sheila. “Now he gets bored if he has to stay around the house. He has great self-esteem. He has a lot more friends, and he goes to the show, he goes bowling, goes driving, goes swimming. Before he went to weight management he wouldn’t do anything.
“It has improved his academics, too,” she says. “He participates more in discussions and is more open with people. He is a really good kid.”
SSM Cardinal Glennon Children’s Medical Center Joins School and Community Partnership
Nutrition, Exercise and Tobacco Issues AddressedThe Missouri Foundation for Health has awarded a grant to SSM Cardinal Glennon Children’s Medical Center and Saint Louis University for a program that will address nutrition, exercise and tobacco usage in the Jennings Public School District.
The Schools and Communities in Partnership Project aims to reduce personal behaviors and environmental factors that contribute to obesity and tobacco usage. The Missouri Foundation for Health provided half the funding for the project. Cardinal Glennon Children’s Medical Center and the university provided matching funds.
The project takes the expertise of the medical center into the community to assist the Jennings School District in formulating health and wellness policies for its students, says Nadim Kanafani, M.D., a pediatric endocrinologist at Cardinal Glennon Children’s Medical Center. The next step will be evaluation of the nutritional, exercise and tobacco environment facing students.
“We will train Jennings volunteers to take clipboards and look at each school – their playgrounds and cafeterias – and the retail environment around each school. We will watch kids eating in the cafeterias. Down the road, as Jennings changes its policies on nutrition, physical activity and tobacco, we will assess outcomes,” says Kanafani, project director for the grant.
“The goals are to have kids eat more fruits and vegetables, have more physical activity and be more aware of and think differently of tobacco. Two other keys are replication and dissemination, taking this experience to other schools and being able to report on what works and doesn’t work.”
Cardinal Glennon Children’s Medical Center and the Jennings School District will collaborate with the Healthy Youth Partnership, which connects more than 80 regional organizations in efforts to reduce obesity. The project will include organizations such as the American Lung Association, which has an ongoing program to reduce tobacco usage by youth.
The project’s first year will cover technical assistance, policy formulation and baseline data collection, Kanafani says. “Year two will focus on how best to implement health and wellness policy.”